Optimizing Colorectal Surgery Recovery: Strategies for Long-Term Success
Enhancing recovery after colorectal surgery and improving long-term health outcomes is a pressing concern at the forefront of modern medical discussions. Optimizing recovery remains a critical step in surgical care. Enhanced Recovery After Surgery (ERAS) protocols offer comprehensive strategies tailored to boost recovery speed and effectiveness. These strategies are crucial for minimizing hospital stays, reducing complications, and improving patients’ quality of life.
Understanding Enhanced Recovery After Surgery (ERAS)
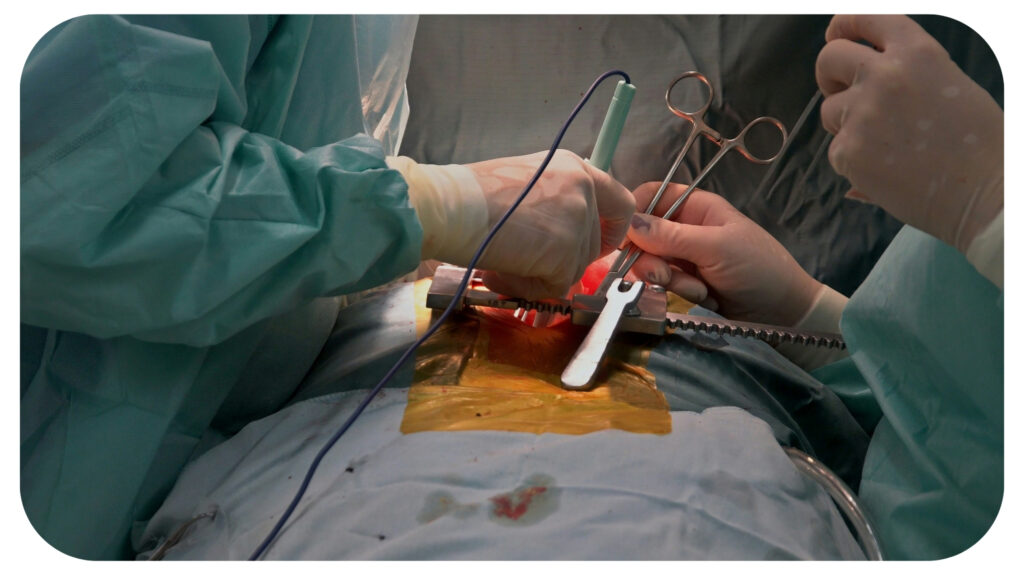
Enhanced Recovery After Surgery (ERAS) protocols are transforming colorectal surgical recovery by targeting all phases of the process—preoperative, intraoperative, and postoperative. With a focus on reducing recovery times and complications while improving outcomes, ERAS provides a structured, patient-centered approach based on evidence-based practices.
Key ERAS components include thorough preoperative education, nutritional support, and optimizing health before surgery. Intraoperatively, surgical and anesthetic techniques aim to reduce tissue trauma, manage pain effectively, and limit the need for opioids, facilitating faster recovery. Postoperative strategies emphasize early mobilization, minimal narcotics, and early nutrition to support healing and prevent complications like blood clots.
Studies affirm ERAS’s effectiveness in shortening hospital stays, lowering complication rates, and improving patient satisfaction. For instance, a 2020 Annals of Surgery study noted a reduction in surgical site infections with ERAS, underscoring its success in optimizing recovery. Adopting ERAS protocols in colorectal surgery not only boosts immediate recovery but supports long-term health, promoting a quicker return to daily life and overall well-being.
Preoperative Strategies for Recovery Optimization
When preparing for colorectal surgery, implementing effective preoperative strategies is crucial to ensure a smooth and swift recovery. Patients stand to benefit significantly from an organized approach that focuses on both physical and mental preparation. Two essential components include nutritional optimization and patient education, both playing vital roles in setting the groundwork for post-surgical recovery.
A robust nutritional plan before surgery can greatly influence recovery outcomes. Instead of the traditional fasting method, modern practices encourage patients to focus on tailored nutrition to support their bodies. One key aspect is carbohydrate loading, which involves ingesting a carbohydrate-rich drink a few hours before surgery. This practice helps maintain energy levels and reduces insulin resistance, ultimately leading to better surgical outcomes and a quicker recovery process.
Avoiding fasting is another critical factor. While fasting was once a standard pre-surgery protocol, current insights suggest maintaining a steady nutrient intake to support bodily functions. This approach prevents the weakening of the immune system and aids in reducing anxiety levels, allowing patients to face surgery with a more resilient body and mind. With these tailored nutritional strategies, patients are better positioned to handle the physiological demands of surgery and heal efficiently.
Empowering patients with knowledge and involvement in their own recovery journey is a cornerstone of successful surgical outcomes. Understanding the entire process, from surgery specifics to post-op expectations, equips patients with a realistic view of what lies ahead. Informed consent is an opportunity for patients to grasp the intricacies of their treatment, ensuring they know their role in the healing process.
“Actively engaging patients in their recovery plan, healthcare providers foster a sense of ownership and control,” says colorectal surgeon and physician Dr. Omar Marar. “This engagement can involve setting recovery goals, learning about pain management options, and understanding the importance of early mobilization.”
Patients who are informed and involved often experience less anxiety, adhere better to postoperative guidelines, and show enhanced motivation to return to daily activities.
The journey to recovery doesn’t start in the operating room; it begins with well-informed, well-prepared patients who are partners in their health care. These preoperative strategies set the stage for a recovery that is quicker and more sustainable in the long run. Paving the way for such proactive measures can indeed alter the trajectory of surgical recovery, making it more effective and patient-centric.
Postoperative Care and Management
Effective postoperative care is essential for optimizing recovery after colorectal surgery. This part of the recovery process focuses on reducing complications and promoting a speedy return to regular activities. Two major components of postoperative care are pain management and early mobilization, both crucial for a successful recovery.
Managing pain without relying too heavily on opioids is a key factor in postoperative care. Multimodal pain management employs a variety of techniques to achieve this. Combining different types of pain relief can help manage discomfort while minimizing the negative effects associated with opioid use. The goal is to provide effective pain relief while avoiding the side effects of opioids, which can include nausea, dizziness, and even addiction. This approach not only helps patients feel better faster but also supports overall healing by enabling them to participate more fully in other elements of their recovery plan.
Getting patients moving soon after surgery is another key strategy in postoperative management. Early mobilization significantly reduces the risk of complications such as blood clots, pneumonia, and muscle weakness, all of which can be setbacks in recovery. Encouraging patients to walk and engage in physical activity as soon as it’s safe can have numerous benefits. Physical therapy often plays a substantial role here. Therapists meet with patients shortly after surgery to develop a mobility plan tailored to their specific needs. This proactive approach acknowledges that movement is medicine, paving the path to a smoother and faster recovery. Mobilization initiatives typically include guided exercises and gradual increases in activity, ensuring patients build confidence alongside their physical strength.
These aspects of postoperative care can make a substantial difference in recovery from colorectal surgery. When focusing on pain management and early movement, patients are equipped to face this crucial phase of healing effectively.
Long-Term Success and Follow-Up Care
Long-term success after colorectal surgery depends on diligent follow-up and lifestyle changes. While patients may wish to return quickly to daily life, ongoing monitoring and adjustments play a key role in recovery and overall health.
Regular follow-up appointments help providers track progress, address issues, and refine treatment as needed. Early detection during these visits prevents complications from escalating. Patients typically follow a structured schedule of office visits, lab tests, and imaging studies, which helps detect issues like infections early and provides reassurance for any ongoing concerns.
Lifestyle changes are equally crucial, supporting recovery through diet, exercise, and routine screening. Adopting healthier habits strengthens recovery, reduces recurrence risk, and improves quality of life.
Enhanced Recovery After Surgery (ERAS) protocols have transformed recovery with a comprehensive approach, emphasizing nutrition, education, pain management, and early mobilization. This strategy leads to shorter hospital stays, fewer complications, and higher satisfaction rates. ERAS’s holistic focus on every recovery phase offers lasting improvements in surgical outcomes, which continue to advance as protocols evolve.
Recommended For You
Why is Back Pain at Night a Red Flag?
Most Inside
Most Inside offers high-quality recommendations and valuable updates to enhance all aspects of your life, providing premium guidance and enriching experiences.




